Evidence Shows Women’s Health and Pain Issues are Taken Less Seriously Than Men’s
 Historically, modern medical research has focused on the health of men, based on statute and tradition. Only in the past 2 to 3 decades, have restrictions that prohibited many women from participating in clinical trials been lifted, allowing researchers to thoroughly and scientifically consider how the health outcomes of women differ from men’s.
Historically, modern medical research has focused on the health of men, based on statute and tradition. Only in the past 2 to 3 decades, have restrictions that prohibited many women from participating in clinical trials been lifted, allowing researchers to thoroughly and scientifically consider how the health outcomes of women differ from men’s.
Due to the way in which women have been shortchanged with regards to the understanding of their health and pain issues, many symptoms women experience were and continue to be misdiagnosed or dismissed by their physicians. Diseases that affect women disproportionately tend to receive a small percentage of funding when compared to diseases that impact the health of men. Research and understanding of common ailments that affect men are decades ahead of research on the same ailments as they affect women, such as heart disease.
The disparities between care offered to men vs. women
There is increasing knowledge available now regarding the inequalities between how women and men are diagnosed and treated in medical settings. Research indicates that doctors and nurses prescribe fewer pain medications to women post-surgery than they do for men. This is despite the fact that women report more frequent episodes of pain and with greater severity. One study performed by the University of Pennsylvania concluded that when visiting an emergency room, women waited 16 minutes longer than men to be given pain medication.
A survey of more than 2,400 women affected by chronic pain revealed that more than 5 out of 6 of these women believed they had experienced some measure of gender discrimination from their healthcare providers. Also, women, unlike men, are sometimes told by medical professionals their pain is influenced by emotional distress, i.e. psychosomatic.
There is an increasing understanding in the medical community that existing bias concerning an entire range of factors has an adverse impact upon the care women receive. However, these treatment disparities between men and women, although present and measurable, are not based on conscious prejudice. At the same time, the potential for medical negligence or malpractice due to the misdiagnosis of women’s conditions is still present.
Why the disparity?
Those who have researched and studied diagnostic errors in the medical arena can tell you that until recently, a large blind spot has existed in the medical community with a failure to systematically track the number of times patients are misdiagnosed and diagnoses are missed. Part of the failure has been due to a lack of feedback given to doctors after they make mistaken diagnoses. Doctors often do not hear if they diagnosed incorrectly unless the patient returns to specifically inform them of the error.
There is a trust and knowledge gap involved with the failures that occur in diagnosing some of the conditions women face. For instance, if a woman actually has an autoimmune disease, the first few doctors she sees may diagnose her has simply experiencing stress or depression. It may only be the last doctor that diagnoses her condition correctly. However, the previous three or four doctors never receive information that informs them that their diagnosis was wrong. This scenario can give some doctors a false sense of their diagnostic capabilities and also reinforce the wrong perception that women are prone to certain symptoms that are simply mental or emotional in nature instead of an actual physiological problem.
Any medical misdiagnosis can potentially constitute medical malpractice, giving the injured party the right to pursue compensation. If this is the situation your face, having an experienced medical malpractice attorney on your side is essential.
Please contact Paulson & Nace, PLLC through this contact form or by calling 202-463-1999.
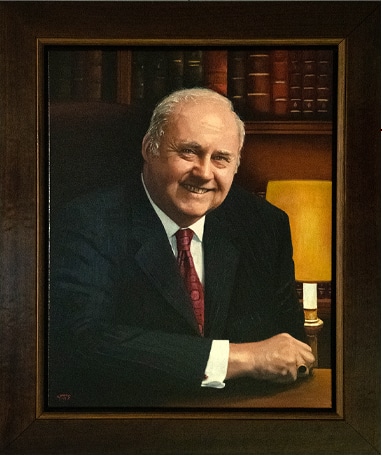
For more than 40 years, Barry J. Nace has worked to protect the rights of victims of medical malpractice and other personal injuries. Throughout his career, he has proven that multimillion-dollar awards are not a matter of luck, but the result of experience, hard work, outstanding trial skills, and an unquestioned dedication to justice. To date, Mr. Nace has produced dozens of verdicts and settlements in excess of $1 million with three in excess of $30 million. Read more about Barry J. Nace.
